Mothers infected with HIV can safely breastfeed their babies as long as they are on medication and the virus is untraceable, according to a pediatricians' organization.
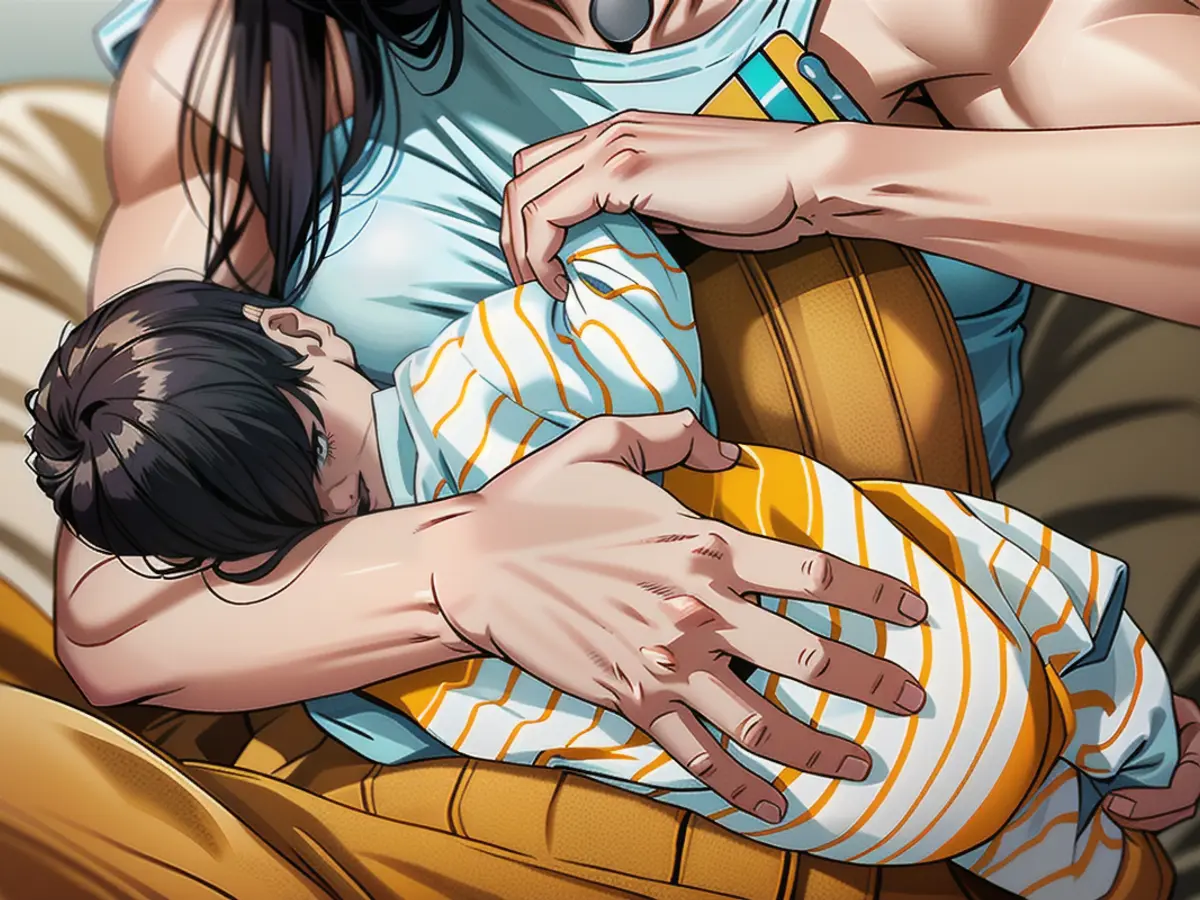
As a mother living with HIV in Colorado, LaTonya considered it essential to capture the moment when she was able to breastfeed her son.
"That's how important it was to me," LaTonya said of the significance of the photos. "I wanted to make sure we had that forever."
Taking a different stance than before, the American Academy of Pediatrics (AAP) now believes people with HIV can breastfeed their infants with "very low" risk if they follow specific guidelines and have support from their healthcare team.
In the past, breastfeeding was strongly discouraged for mothers with HIV, and it was only recommended that they use formula or certified, banked donor human milk instead. However, the new clinical report from AAP published in the journal Pediatrics suggests that healthcare professionals should provide counseling to mothers who wish to breastfeed while receiving antiretroviral treatment (ART) as prescribed and maintaining an undetectable amount of the virus in their body.
This contrasts with the standard recommendation that women with HIV in the United States avoid breastfeeding. The recommendation against breastfeeding for people with HIV was made in the 1980s by the US Centers for Disease Control and Prevention (CDC).
"The AAP recommends that for people with HIV in the United States, replacement feeding (with formula or certified, banked donor human milk) is the only option that is 100% certain to prevent postnatal transmission of HIV," the report says. "However, pediatric health care professionals should be prepared to provide infant feeding counseling and a family-centered, culturally sensitive, harm reduction approach for people with HIV on ART with sustained viral suppression who desire to breastfeed."
HIV is a virus that attacks the body's immune system and can develop into acquired immunodeficiency syndrome (AIDS) if left untreated. LaTonya has been living with HIV for around 20 years but knew she wanted to breastfeed her son because of the many health benefits it offers infants.
"Breastfeeding is such a fantastic thing for babies. It's associated with a lower risk of asthma, obesity, type 1 diabetes, and sudden infant death syndrome," she said. "As a mom, you just want to give your child the best shot at becoming the best person they can be. And breastfeeding was a step for me to be able to provide that for him."
LaTonya consulted with her doctors about her decision and together, they came up with a plan. Her viral load is undetectable and she is taking antiretroviral drugs, making it possible for her to breastfeed.
"We discussed constant monitoring of viral loads to ensure there wasn't a spike in her viral load and that complete adherence to medication was essential," LaTonya explained.
LaTonya acknowledged the importance of understanding the science behind it and explained that, if you're undetectable, you cannot transmit the virus to your partner. The same goes for adhering to medication, as it won't transfer through the breast milk to your child.
"The risk of HIV transmission through breast milk is highest in the baby's first four to six weeks of life, ranging between 5% and 6%, but the risk is estimated to be less than 1% for women with undetectable viral loads and taking antiretroviral medications," Abuogi said. Dr. Lisa Abuogi, the lead author of the report and a pediatrician in Colorado who works with people with HIV during their pregnancies, further explained the significant shift in the AAP's stance on breastfeeding.
"What's new is that the AAP is explicitly saying that pregnant people with HIV who are on treatment can be supported to breastfeed," Abuogi added. "This has been a long evolution, and people living with HIV have been a part of advocating for this change."
Throughout the years, people living with HIV have felt shame or distress due to the inability to breastfeed, worrying about revealing their HIV status within their communities. Now, women have the choice to decide whether they want to breastfeed, and this empowering option is being embraced by healthcare professionals.
Estimated to be around 5,000, the number of people with HIV giving birth in the United States each year highlights the importance of providing the same infant-feeding options for them.
In 2021, an advisory group to the US Department of Health and Human Services adjusted their suggestions on infant feeding, asserting that individuals with HIV, who are on antiretroviral therapy (ART) and have sustained undetectable viral loads, can breastfeed if they choose to.
The new position of the American Academy of Pediatrics (AAP) aligns with the recommendations from this HHS panel. Rana Chakraborty, a pediatric infectious disease specialist and researcher at the Mayo Clinic in Minnesota, a member of the HHS' Panel on Treatment of HIV During Pregnancy and Prevention of Perinatal Transmission, commented on this development.
"The process of discussing this has been ongoing for a few years," said Chakraborty, who wasn't involved in the AAP's new report. "The authors of the AAP report have done a nice job summarizing the US's current national guidelines."
Chakraborty explained how research from various investigators, including many from the United States working in resource-poor settings, has supported the idea of breastfeeding safely when the mother is taking antiretroviral therapy and maintaining undetectable HIV viral loads. "Breastfeeding during HIV infection does, however, require a multidisciplinary team to ensure the safety of both the mother and child."
The AAP's recommendations indicate a consensus among leading medical organizations that mothers living with HIV should be supported and counseled in their decision to breastfeed their infants, according to Elaine Abrams, a professor of epidemiology and pediatrics at the Columbia University Medical Center in New York.
"The same message is coming from all the bodies that provide guidelines to clinicians," Abrams said. "This represents a consensus, and it puts the mother at the center of the conversation and decision-making."
Abrams emphasized that the shift is from telling the mother what to do to understanding her desires, providing her with evidence and information, and supporting her in her choice. "In the past, that wasn't always the case."
During the early 2000s, studies revealed that infants born to women with HIV in low-income countries had higher risks of illness and death when fed formula. This was linked to contaminated water sources used for mixing the formula. As a result, the World Health Organization suggested that HIV-positive mothers in places without safe drinking water and accessible formula should breastfeed their babies.
Subsequent research discovered that when mothers took ART or infants received preventive antiretrovirals, the risk of HIV transmission decreased. The AAP report remarked that a consensus on the optimum regimen of preventive antiretrovirals for infants during breastfeeding is not yet established. Furthermore, individuals breastfeeding were advised to do so exclusively since mixing breastfeeding with formula or solid foods has been associated with increased HIV transmission. The AAP report suggested that this increased transmission rate is due to disrupted infant gut integrity from consuming things other than human milk, reduced levels of antiviral or anti-inflammatory substances found in breast milk, or other potential mechanisms.
LaTonya, who breastfed her HIV-positive child, shared guidance from her medical team regarding the need to exclusively breastfeed and not mix formula or solid foods. "If we were going to breastfeed, that's all we could do."
In addition to counseling and supporting mothers seeking to breastfeed, the AAP encouraged routine HIV testing for pregnant women and linking people living with HIV or newly diagnosed to treatment in the new recommendations.
LaTonya hopes that the AAP's new stance will inspire healthcare providers to educate the public more extensively about the meaning of an undetectable HIV level, how infections can be treated, and how the virus can be suppressed. "This is something that they live with, and it's not something to be afraid of," she said. "I believe that is largely due to a lack of education." National HIV testing, LaTonya suggested, could be an ideal opportunity for doctors to have educational discussions with their patients.
Read also:
- No food or coffee for three days, just juice, juice, juice instead: a field report
- How to get rid of the flu if you have caught it
- Doctors warn of penis fractures and other injuries during the Christmas season
- Corona or flu epidemic? These pathogens are making us cough and sniffle right now
After the American Academy of Pediatrics (AAP) changed their stance on breastfeeding for mothers with HIV, LaTonya, a mother living with HIV in Colorado, was able to safely breastfeed her son.
Adhering to specific guidelines and having the support of her healthcare team, LaTonya was able to maintain an undetectable amount of the virus in her body, making it safe for her to breastfeed.
Source: edition.cnn.com