Should one consider undergoing a mammogram at the age of 40?
This new advice from the task force contrasts with their former recommendations, which called for biennial mammograms at the age of 50. For women in their 40s, they advised discussing the decision with their healthcare provider, but there was no specific guidance to start until they reached 50.
I wanted to delve deeper into these updates. Who should abide by these revised suggestions? Are there women that may need screening even earlier or more frequently? What other tests besides mammograms could be necessary? And, what preventive measures can be taken to lower the risk of developing breast cancer?
To address these questions, I sought out CNN's wellness expert, Dr. Leana Wen. An emergency physician and adjunct associate professor at George Washington University, Wen has previously served as the health commissioner in Baltimore.
CNN: How often does breast cancer occur?
Dr. Leana Wen: In the USA, breast cancer is the second most common cancer in women and it is the second leading cause of cancer death among women. The American Cancer Society states that one out of every eight women will be diagnosed with invasive breast cancer in their lifetime. Each year, about 42,000 women pass away from this cancer.
It's crucial for women to be aware of their risk factors and get screened accordingly. Screening is when tests are performed before any symptoms surface. Early detection through screening increases the chances of catching cancers before they spread and significantly improves the potential for effective treatment.
CNN: Why did the US Preventive Task Force make these alterations?
Wen: There has been a troubling uptick in cancer diagnoses among younger individuals. The same trend is observed with colon cancer as well as breast cancer.
Breast cancer is the most commonly diagnosed cancer and is the leading cause of cancer death in women between the ages of 20 and 49. Younger women usually have more aggressive cancers when they are diagnosed compared to older women.
This holds particularly true for Black women. The death rate from breast cancer in Black women in their 40s was 27 per 100,000 person-years, compared to 15 per 100,000 person-years among White women, according to a 2023 JAMA Network Open study.
A study from the Lancet Oncology discovered that the mortality from breast cancer could be reduced by starting mammograms at age 40.
The US Preventive Task Force's modification now aligns its recommendations with those of other major national organizations. The American College of Obstetricians and Gynecologists suggests screening every one or two years commencing at age 40 and continuing until at least age 75. The American Cancer Society gives women aged 40 to 44 the option to get a mammogram yearly and recommends those 45 and over to have annual mammograms. (People over 55 can switch to every other year or continue annual mammograms.)
CNN: Precisely, who should follow these new suggested timelines?
Wen: I suggest women pay close attention to these updated guidelines and discuss them with their physicians. This advice is intended for women with an average breast cancer risk. Women at average risk should begin mammograms by the age of 40.
This advice does not apply to people with an elevated risk. Everyone needs to assess their own risk to determine if they may require additional tests and more frequent screenings.
The new guidance also pertains to individuals assigned female at birth, which encompasses not only cisgender women but also transgender men and nonbinary individuals. These persons should also hold conversations with their healthcare providers to discuss their risk factors and how frequently they should receive screenings.
CNN: How do women figure out if they require more frequent or earlier screenings?
Wen: The most significant factor is personal or family history of breast cancer. People with a history of breast cancer in their past need to consult their oncologist or primary care doctor to determine the necessary testing and frequency for monitoring cancer recurrence. The same goes for individuals who received prior radiation to the chest for different cancers.
Family history is also a key factor in determining risk. Women with a sister, mother, or other close relative who had breast cancer have double the average risk of developing breast cancer. Women with two first-degree relatives have five times the risk.
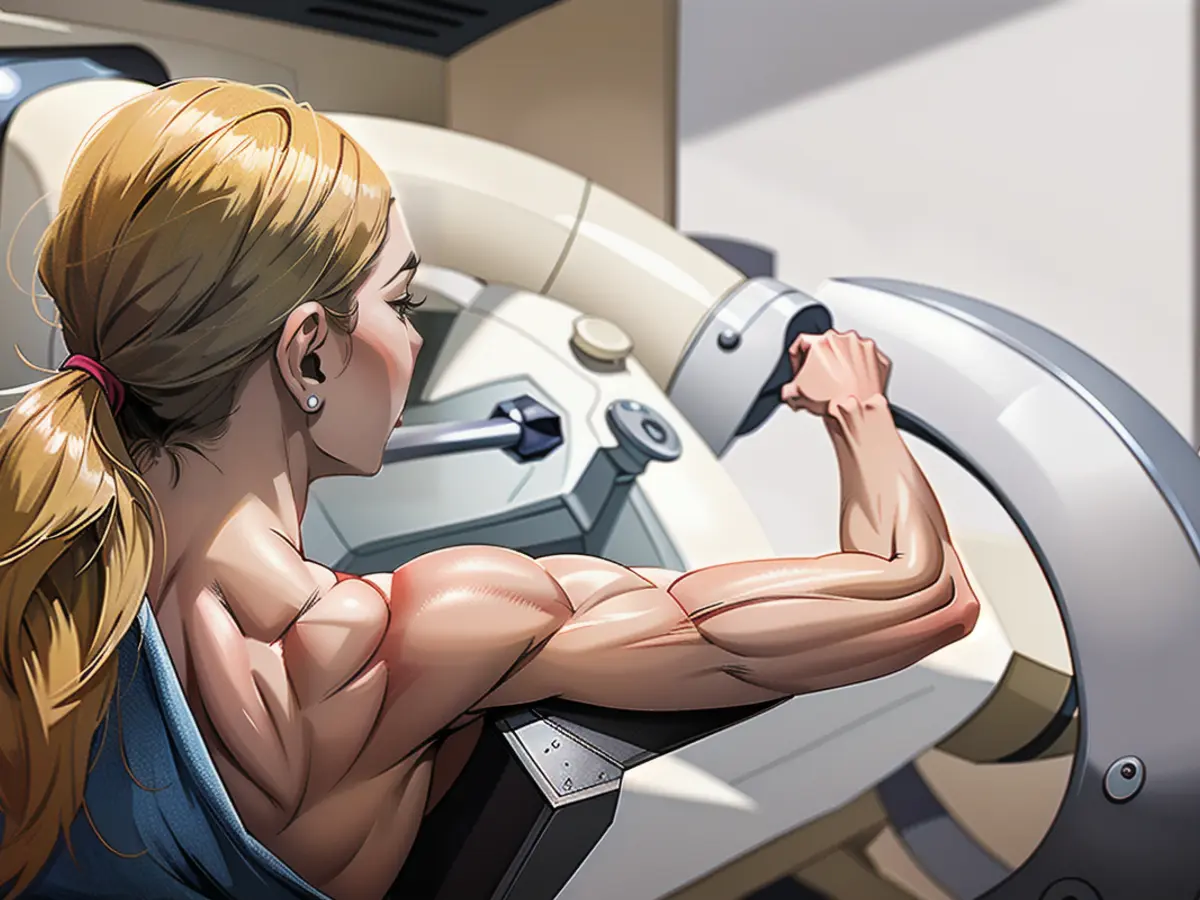
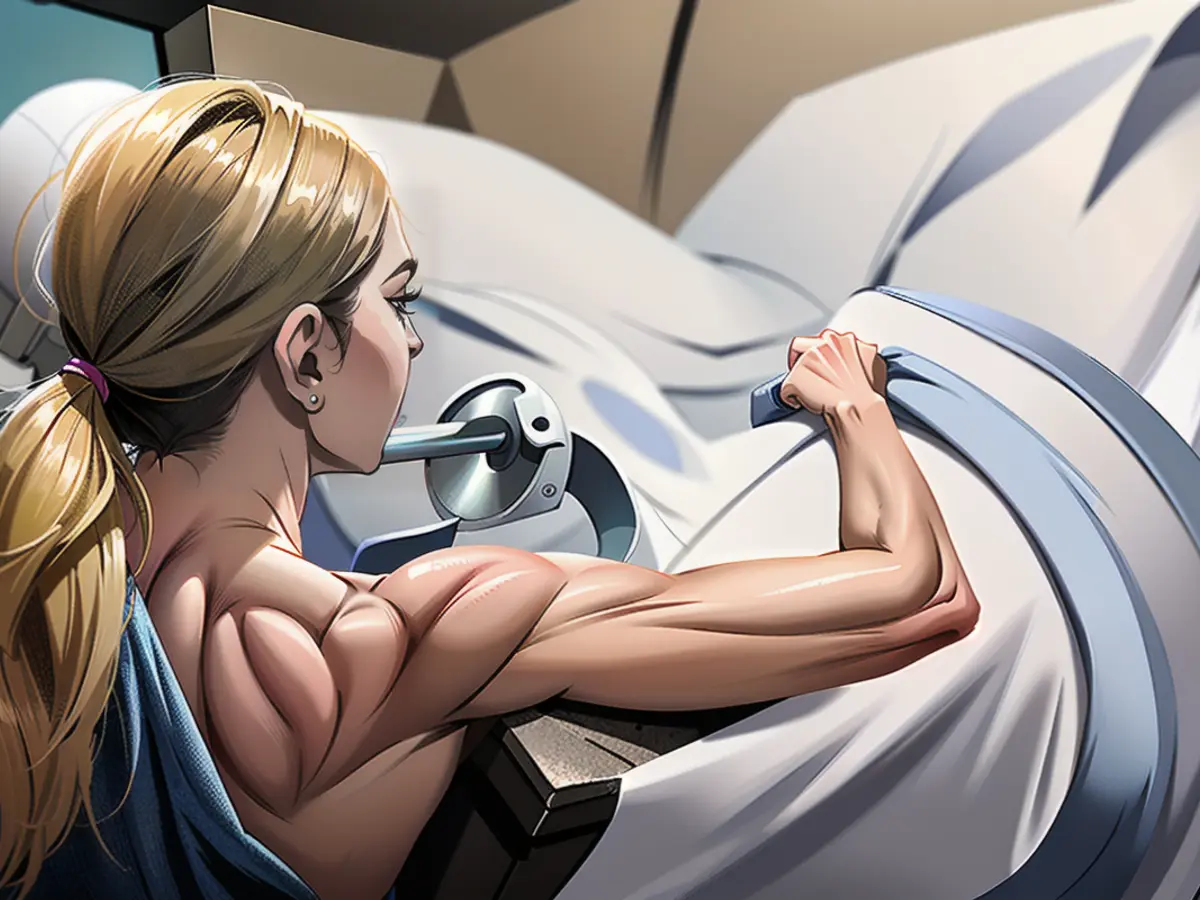
CNN: How will women experience their first mammogram?
Wen: A mammogram is an x-ray of the breasts. The process generally involves the technician guiding you to a room where you remove your bra and shirt, wipe off any deodorant from your armpit area that could affect the results, and change into a gown that only covers you from the waist up (you do not need to remove your underwear, pants, or shoes).
The section of the mammogram that may cause discomfort is when the technician positions your breasts between two plastic imaging plates that apply pressure during the image capture. However, the discomfort is usually very brief. To alleviate concerns about potential discomfort, one could consider taking Tylenol or ibuprofen an hour prior to the mammogram.
An individual with a genetic history of breast cancer might be advised to undergo genetic testing. Those at a higher risk of breast cancer may require mammograms at an earlier age or more frequently. Furthermore, other tests, such as breast ultrasounds, breast MRIs, or both, may complement mammograms in certain circumstances.
Now, there are professionals who endorse additional testing for women with average risk and dense breast tissue. While mammography is still the primary screening tool, these women may require additional imaging to spot potential masses more accurately.
The American College of Radiology, for instance, suggests a breast MRI for some women with intermediate risk and dense breast tissue. However, the US Preventive Services Task Force has not yet endorsed this advice, which could affect insurance coverage for imaging. Women who are concerned about their breast cancer risk should consult their physicians to determine the best approach based on their individual and family medical histories and whether they're willing to bear any extra expenses.
CNN: Can you explain why women over 74 should no longer undergo breast cancer screenings?
Wen: The US Preventive Services Task Force states that there is not enough evidence to suggest for or against mammograms for women aged 75 years or older. Nevertheless, other major medical organizations persist in recommending mammograms for individuals in this age group, particularly if they are in good health and have a long life expectancy. As always, this is a topic to be discussed with your healthcare provider, who can evaluate your overall health and consider your preferences.
CNN: Are there steps younger people can take to reduce their cancer risk?
Wen: Breast cancer risk factors include tobacco use and excessive alcohol consumption, so quitting smoking and reducing alcohol intake can help lower the risk. Scientific studies suggest that exercise can reduce the risk of cancer in general, and following a diet high in whole foods while minimizing consumption of highly processed foods can also make a difference.
Women should also consult their doctors if they notice any worrying symptoms, such as a new lump or mass in their breast or underarm, redness or scaly skin on their breasts, nipple discharge other than breast milk, or pain or swelling in their breasts.
Read also:
- No food or coffee for three days, just juice, juice, juice instead: a field report
- How to get rid of the flu if you have caught it
- Doctors warn of penis fractures and other injuries during the Christmas season
- Corona or flu epidemic? These pathogens are making us cough and sniffle right now
The revised recommendations suggest that women with average breast cancer risk should start getting mammograms at the age of 40. This advice does not apply to individuals with an elevated risk, who may require additional tests and more frequent screenings.
For Black women in their 40s, the death rate from breast cancer is higher than that of White women, making it crucial for them to be aware of their risk factors and get screened accordingly.
Source: edition.cnn.com